New Diagnosis/Overwhelmed
New Diagnosis/Overwhelmed
Hi.
I may be on here too early - because I don't know much yet - but I am trying to read things online and I'm feeling very scared and overwhelmed. I guess I'm still in shock.
I had a colonoscopy last Monday. I had blood in my stool since last September (6 mos. ago) but was told it was a hemorrhoid by my GYN and then it was an anal fissure by a ColoRectal MD - so it took me until recently (too long!) to get a colonoscopy. Anyway, she found two polyps and removed one. The other was large so she left it and had it sent for pathology. It came back positive. All I know is that it's in my rectum and it's 6cm (she described it as "large" and I'm assuming large = well established = far along = very bad).
My doctor's office made my very first appt with my local cancer center on Thursday (it's Spring Break here so many doctors are away). The doctor is not board certified and my cousin (a radiologist) says I should (1) only see a board certified person and (2) consider traveling to a top cancer care center.
My questions....
- Is it worth it to see this doctor just to get the ball rolling (Scans or whatever)? Or would it be worth it to wait another (5-7?) days to see another doctor in the same hospital who may be back the following week? Once the ball is rolling, can you just switch gears with other doctors and treatment options?
- What is the process and how long does it take to see doctors in major care facilities (NYC, Boston, Cleveland, Baltimore are all within 4-6 hours from me)? I've already read articles on things to consider when traveling for cancer treatment so I am aware of some of the things you need to think about but just can't imagine traveling when you're that sick.
- I have not yet called my insurance company. Any advice there?
I realize that I don't know have specific info yet but given the size of my polyp and it's proximity to my anus, I'm assuming this won't be an easy one (as if cancer ever is easy). I have read the post on questions to ask your doctor - very helpful - thank you.
I have read many posts on here and you all have so much clinical knowledge. I assume you pick that up as you go in your cancer journey.
Thanks so much for all your help.
49 - Female
DX: RC
Size: 6cm near (?) anus
I may be on here too early - because I don't know much yet - but I am trying to read things online and I'm feeling very scared and overwhelmed. I guess I'm still in shock.
I had a colonoscopy last Monday. I had blood in my stool since last September (6 mos. ago) but was told it was a hemorrhoid by my GYN and then it was an anal fissure by a ColoRectal MD - so it took me until recently (too long!) to get a colonoscopy. Anyway, she found two polyps and removed one. The other was large so she left it and had it sent for pathology. It came back positive. All I know is that it's in my rectum and it's 6cm (she described it as "large" and I'm assuming large = well established = far along = very bad).
My doctor's office made my very first appt with my local cancer center on Thursday (it's Spring Break here so many doctors are away). The doctor is not board certified and my cousin (a radiologist) says I should (1) only see a board certified person and (2) consider traveling to a top cancer care center.
My questions....
- Is it worth it to see this doctor just to get the ball rolling (Scans or whatever)? Or would it be worth it to wait another (5-7?) days to see another doctor in the same hospital who may be back the following week? Once the ball is rolling, can you just switch gears with other doctors and treatment options?
- What is the process and how long does it take to see doctors in major care facilities (NYC, Boston, Cleveland, Baltimore are all within 4-6 hours from me)? I've already read articles on things to consider when traveling for cancer treatment so I am aware of some of the things you need to think about but just can't imagine traveling when you're that sick.
- I have not yet called my insurance company. Any advice there?
I realize that I don't know have specific info yet but given the size of my polyp and it's proximity to my anus, I'm assuming this won't be an easy one (as if cancer ever is easy). I have read the post on questions to ask your doctor - very helpful - thank you.
I have read many posts on here and you all have so much clinical knowledge. I assume you pick that up as you go in your cancer journey.
Thanks so much for all your help.
49 - Female
DX: RC
Size: 6cm near (?) anus
Female - RC dgns @ 49 y
Adenocarcinoma
10-11 cm from anal verge ("large")
Stage 3a - T4N0M0
FOLFOX May -Sept 18
Capecetabine + Radiation - 28 sessions - Oct - Nov 18
Jan 19 - MRI & flex sig show tumor gone, Chest/ab CT no change
Feb 19 - MRI & flex sig show tumor gone
W&W (must travel)
.....W&W surveillance 2019,2020,2021,2022,2023....
Jan 24 - approaching 5 years this Spring with W&W surveillance to end.
*grateful*
Adenocarcinoma
10-11 cm from anal verge ("large")
Stage 3a - T4N0M0
FOLFOX May -Sept 18
Capecetabine + Radiation - 28 sessions - Oct - Nov 18
Jan 19 - MRI & flex sig show tumor gone, Chest/ab CT no change
Feb 19 - MRI & flex sig show tumor gone
W&W (must travel)
.....W&W surveillance 2019,2020,2021,2022,2023....
Jan 24 - approaching 5 years this Spring with W&W surveillance to end.
*grateful*
-
weisssoccermom
- Posts: 5988
- Joined: Thu May 10, 2007 2:32 pm
- Location: Pacific NW
Re: New Diagnosis/Overwhelmed
First of all, welcome to the forum. I know you would rather not be here but here you are. Second of all, don't assume that because the polyp is big it necessarily means the worst case scenario. It isn't the size of the polyp, but rather the DEPTH of the tumor in the rectal wall that is one factor determining what stage you are. Many people have tiny tumors/polyps but there cancer has spread via the lymphatic or vascular system making them a stage III/IV while others with larger (or small) tumors end up being a stage I. For example, I had a 4cm X 6cm tumor located in my rectum but was staged as a stage IIA. SO, being large does NOT necessarily equate with being 'well established' or 'far along' or 'very bad'.
You don't say what type of doctor you have an appointment with. Is the doctor a surgeon? If so, then I would want to see a board certified colorectal surgeon as opposed to a general surgeon for rectal cancer (which I am assuming yours is based on your description). However, that doesn't mean that you can't start by seeing an oncologist first. Honestly, with rectal cancer, your first steps will likely be to see an oncologist who will get the ball rolling with testing....and EUS (endorectal ultrasound) to determine the depth the tumor has penetrated the rectal wall and to visualize the local nodes, a CT or MRI to check the lungs, liver, abdomen, kidneys, etc. for any signs of distant nodes or other potential mets and some blood work. In addition, you will likely be sent to a radiation oncologist to get the process started to undergo radiation to help shrink the tumor. You can start with a surgeon but honestly, he/she won't be doing anything other than to refer you for testing. IF you have a good relationship with your GP, have him/her start the process by ordering a CEA (blood test) and a CBC/CHEM panel. That same doctor can also order a chest/abdomen/pelvic CT with contrast to also start the process.
As for going to a major cancer center.....wait until you have more information. Honestly, those who are early stages don't necessarily need to be seen at a major cancer center, especially not for the chemo and/or radiation as it is pretty much standard of care no matter where you are. However, if you are further along, then, IMO, you may want to consider setting up an appointment at one of these places. As for calling your insurance company, you don't have any reason to. You don't have a treatment plan and there's nothing to be accomplished by calling them.
My advice.....call your GP and ask him/her to start the process going by ordering the bloodwork and CT with contrast. Get an appointment with an oncologist and IF you want to see a surgeon now, fine, but wait for the board certified colorectal surgeon. Remember that all surgeons are board certified in GENERAL SURGERY but not all are certified in COLON AND RECTAL surgery. There is no reason with rectal cancer to necessarily see the surgeon first. He/she isn't going to operate first unless there is an emergent situation and they don't Rx the chemo. While a surgeon may refer you to a radiation oncologist, you will still need to be referred to and seen by an medical oncologist to get the chemo Rxd. Get in with the onc first to get things going and then see the surgeon.
Best of luck.
You don't say what type of doctor you have an appointment with. Is the doctor a surgeon? If so, then I would want to see a board certified colorectal surgeon as opposed to a general surgeon for rectal cancer (which I am assuming yours is based on your description). However, that doesn't mean that you can't start by seeing an oncologist first. Honestly, with rectal cancer, your first steps will likely be to see an oncologist who will get the ball rolling with testing....and EUS (endorectal ultrasound) to determine the depth the tumor has penetrated the rectal wall and to visualize the local nodes, a CT or MRI to check the lungs, liver, abdomen, kidneys, etc. for any signs of distant nodes or other potential mets and some blood work. In addition, you will likely be sent to a radiation oncologist to get the process started to undergo radiation to help shrink the tumor. You can start with a surgeon but honestly, he/she won't be doing anything other than to refer you for testing. IF you have a good relationship with your GP, have him/her start the process by ordering a CEA (blood test) and a CBC/CHEM panel. That same doctor can also order a chest/abdomen/pelvic CT with contrast to also start the process.
As for going to a major cancer center.....wait until you have more information. Honestly, those who are early stages don't necessarily need to be seen at a major cancer center, especially not for the chemo and/or radiation as it is pretty much standard of care no matter where you are. However, if you are further along, then, IMO, you may want to consider setting up an appointment at one of these places. As for calling your insurance company, you don't have any reason to. You don't have a treatment plan and there's nothing to be accomplished by calling them.
My advice.....call your GP and ask him/her to start the process going by ordering the bloodwork and CT with contrast. Get an appointment with an oncologist and IF you want to see a surgeon now, fine, but wait for the board certified colorectal surgeon. Remember that all surgeons are board certified in GENERAL SURGERY but not all are certified in COLON AND RECTAL surgery. There is no reason with rectal cancer to necessarily see the surgeon first. He/she isn't going to operate first unless there is an emergent situation and they don't Rx the chemo. While a surgeon may refer you to a radiation oncologist, you will still need to be referred to and seen by an medical oncologist to get the chemo Rxd. Get in with the onc first to get things going and then see the surgeon.
Best of luck.
Dx 6/22/2006 IIA rectal cancer
6 wks rad/Xeloda -finished 9/06
1st attempt transanal excision 11/06
11/17/06 XELOX 1 cycle
5 months Xeloda only Dec '06 - April '07
10+ blood clots, 1 DVT 1/07
transanal excision 4/20/07 path-NO CANCER CELLS!
NED now and forever!
Perform random acts of kindness
6 wks rad/Xeloda -finished 9/06
1st attempt transanal excision 11/06
11/17/06 XELOX 1 cycle
5 months Xeloda only Dec '06 - April '07
10+ blood clots, 1 DVT 1/07
transanal excision 4/20/07 path-NO CANCER CELLS!
NED now and forever!
Perform random acts of kindness
Re: New Diagnosis/Overwhelmed
Just as a follow up, I saw my surgeon first after my tumor was discovered. I was referred to him by my GI doc. He is a board certified colon and rectal surgeon and has tons of experience with this stuff. He referred me to my oncologist who I liked so I stuck with him. He also referred me to my endoscopic ultrasound and explained the staging system to me. So it’s not necessarily true that your surgeon can’t be helpful in this area. Just depends on the surgeon.
40 year-old female
May 2017: Dx rectal cancer T3N2M0
MSS, KRAS G12D
6/17: 28 days chemorad
9/17: LAR/loop ileostomy, CAPOX six rounds
3/18: reversal
9/18: liver met, resection/HAI pump, 11 rounds 5FU, 1 round FUDR
11/19 - local recurrence, brachytherapy, 3 weeks targeted radiation
12/21 - end colostomy
May 2017: Dx rectal cancer T3N2M0
MSS, KRAS G12D
6/17: 28 days chemorad
9/17: LAR/loop ileostomy, CAPOX six rounds
3/18: reversal
9/18: liver met, resection/HAI pump, 11 rounds 5FU, 1 round FUDR
11/19 - local recurrence, brachytherapy, 3 weeks targeted radiation
12/21 - end colostomy
Re: New Diagnosis/Overwhelmed
Hello and thank you so much for your replies with so much advice. The appt Thursday is with a surgeon who specializes in colon and rectal surgery. It says he is a member of a surgical oncology association but it's not clear if he's an oncologist (I assume not). The other doctor (who is board certified but out of town this week) is the same - primarily a surgeon with specialties in colo-rectal area. Both are in same dept of surgery at a teaching hospital. I will call my GP on Monday and inquire about the tests. Thanks again for your advice and time!
Female - RC dgns @ 49 y
Adenocarcinoma
10-11 cm from anal verge ("large")
Stage 3a - T4N0M0
FOLFOX May -Sept 18
Capecetabine + Radiation - 28 sessions - Oct - Nov 18
Jan 19 - MRI & flex sig show tumor gone, Chest/ab CT no change
Feb 19 - MRI & flex sig show tumor gone
W&W (must travel)
.....W&W surveillance 2019,2020,2021,2022,2023....
Jan 24 - approaching 5 years this Spring with W&W surveillance to end.
*grateful*
Adenocarcinoma
10-11 cm from anal verge ("large")
Stage 3a - T4N0M0
FOLFOX May -Sept 18
Capecetabine + Radiation - 28 sessions - Oct - Nov 18
Jan 19 - MRI & flex sig show tumor gone, Chest/ab CT no change
Feb 19 - MRI & flex sig show tumor gone
W&W (must travel)
.....W&W surveillance 2019,2020,2021,2022,2023....
Jan 24 - approaching 5 years this Spring with W&W surveillance to end.
*grateful*
-
retiredteacher
- Posts: 115
- Joined: Sat Oct 21, 2017 1:34 pm
Re: New Diagnosis/Overwhelmed
Be sure your docs do the initial ultrasounds and/or MRIs - in addition to your biopsy - to determine your initial staging. This will ensure you do get appropriate care and are not undertreated or overtreated down the road. Get the best surgeon you can - from a high volume well rated teaching hospital. The confidence and skills will make a difference. You can go local for oncology and radiation - just be sure they are following standards ...
RC F 63 9/17
Adeno 7 cm MSS G2 PET
T3N0M0
2.5K Cap/RT x 25
"Near complete response" PET 1/18
CEA 0.5 10/17, 0.6 10/18
MRI 2/18 yT2N0 12 cm fr AV 3 cm
LAR 2/18 yT1N0M0 0/21 G1 0.3 cm
CAPEOX 3/18, reduced to 80% at cycle 3
Completed 4 cycles; stopped, gut issues, liver enzymes
CT/ colonoscopy 11/18 NED
4/19 NED Sacral fractures/osteoporosis
"Caregiver" to the Iron Man
Hubby CRC Stage 3 2004 NED, Small Cell Lung Cancer Limited 2011 NED, Non-small Cell Lung Cancer 2019 NED October 2019
Adeno 7 cm MSS G2 PET
T3N0M0
2.5K Cap/RT x 25
"Near complete response" PET 1/18
CEA 0.5 10/17, 0.6 10/18
MRI 2/18 yT2N0 12 cm fr AV 3 cm
LAR 2/18 yT1N0M0 0/21 G1 0.3 cm
CAPEOX 3/18, reduced to 80% at cycle 3
Completed 4 cycles; stopped, gut issues, liver enzymes
CT/ colonoscopy 11/18 NED
4/19 NED Sacral fractures/osteoporosis
"Caregiver" to the Iron Man
Hubby CRC Stage 3 2004 NED, Small Cell Lung Cancer Limited 2011 NED, Non-small Cell Lung Cancer 2019 NED October 2019
- susie0915
- Posts: 945
- Joined: Wed Aug 02, 2017 8:17 am
- Facebook Username: Susan DeGrazia Hostetter
- Location: Michigan
Re: New Diagnosis/Overwhelmed
When the GI told me he discovered what he thought was cancer during my colonoscopy, he had already scheduled an appointment the next day with a colorectal surgeon. When I saw the surgeon, after examining me he ordered the ct scan for 2 days later on Sunday and the endoscopic ultrasound Monday. He also scheduled appointments for me to see a oncologist and radiation oncologist. The ct scan showed no metastasis and based on the endoscopic ultrasound was staged 2A rectal cancer. At the same time, I made an appointment for a second opinion at another hospital with a colorectal surgeon. The nurse navigator at the hospital also made appointments with an oncologist and radiation oncologist. I met with all doctors from both hospitals and decided to have treatment at the second hospital. Treatment was going to be the same at both hospitals, but I felt more comfortable with the oncologist at the second hospital, as well as, the coordination of the doctors. Being stage 2A, treatment is pretty standard but it doesn't hurt to seek another opinion. At first I just wanted to get started with treatment, but getting a second opinion gave me peace of mind and didn't really set me back. Even if you have your staging done, you can take the cd's to the second opinion doctors as I did and they will review to determine your treatment plan.
58 yrs old Dx @ 55
5/15 DX T3N0MO
6/15 5 wks chemo/rad
7/15 sigmoidoscopy/only scar tissue left
8/15 PET scan NED
9/15 LAR
0/24 nodes
10/15 blockage. surgery,early ileo rev, c-diff inf
12/15 6 rds of xelox
5/16 CT lung scarring/inflammation
9/16 clear colonoscopy
4/17 C 4mm lung nod
10/17 pel/abd CT NED
11/17 CEA<.5
1/18 CT/Lung no change in 4mm nodule
5/18 CEA<.5, CT pel/abd/lung NED
11/18 CEA .6
5/19 CT NED, CEA <.5
10/19 Clear colonscopy
11/19 CEA <.5
5/15 DX T3N0MO
6/15 5 wks chemo/rad
7/15 sigmoidoscopy/only scar tissue left
8/15 PET scan NED
9/15 LAR
0/24 nodes
10/15 blockage. surgery,early ileo rev, c-diff inf
12/15 6 rds of xelox
5/16 CT lung scarring/inflammation
9/16 clear colonoscopy
4/17 C 4mm lung nod
10/17 pel/abd CT NED
11/17 CEA<.5
1/18 CT/Lung no change in 4mm nodule
5/18 CEA<.5, CT pel/abd/lung NED
11/18 CEA .6
5/19 CT NED, CEA <.5
10/19 Clear colonscopy
11/19 CEA <.5
-
weisssoccermom
- Posts: 5988
- Joined: Thu May 10, 2007 2:32 pm
- Location: Pacific NW
Re: New Diagnosis/Overwhelmed
Check the link below to verify that your surgeon is indeed board certified in colon/rectal surgery.
www.abcrs.org/verify-a-physician-2/
Just because a surgeon 'specializes' in a particular area doesn't mean that he/she doesn't do other types of surgery. In addition, being a surgical oncologist doesn't necessarily mean that the surgeon is anything more than a general surgeon who 'specializes' in cancer surgery. I'm NOT saying that is a negative thing....just saying that, IMO, a patient who has rectal cancer should seek the expertise of a board certified colon/rectal surgeon. I've been a member of this board for over 11 years and have seen, myself included, too many patients who have believed that they were seeing a 'specialist' who was nothing more than a general surgeon who does a lot of colon/rectal surgeries. I'm not implying that that is necessarily a negative thing, BUT....remember that the pelvis is a tight space and, again IMO, needs a specialist....one who has undergone extensive training and one who ONLY operates on the colon/rectum.
You certainly can start out with a surgeon who will almost certainly refer you to an oncologist to get all the testing started although he/she (surgeon) may refer you for the ultrasound. You should also realize that in most cases, you won't actually be dealing with the surgeon until after chemoradiation is over (first he has to start....after testing...at a minimum that is a 2 week process) and after that a minimum of a 6-8 week rest period. Personally, I didn't like the surgeon that I had first met but didn't even think of looking for a second one without first seeing the onc (whom I liked) and getting started with the treatment. My point is that you have time to find a surgeon and you may not feel comfortable or have trust in the first one you see. One thing with rectal cancer is that after diagnosis, it seems to take a whole lot longer than one expected to get started. There are all the tests that need to be done before treatment (usually chemoradiation is first) and it can be very overwhelming and stressful.
Verify the surgeon(s) that you are considering. Get a referral to an oncologist (ask your GP, cousin, friends ...especially nurses) and see him/her to get started. Whichever path you choose to start on just remember that you have to feel comfortable and trust the docs that you are putting your faith in. Your oncologist will be your doctor that you see for most of the next 5-7 years so make sure you like him/her and feel comfortable with his/her judgement.
www.abcrs.org/verify-a-physician-2/
Just because a surgeon 'specializes' in a particular area doesn't mean that he/she doesn't do other types of surgery. In addition, being a surgical oncologist doesn't necessarily mean that the surgeon is anything more than a general surgeon who 'specializes' in cancer surgery. I'm NOT saying that is a negative thing....just saying that, IMO, a patient who has rectal cancer should seek the expertise of a board certified colon/rectal surgeon. I've been a member of this board for over 11 years and have seen, myself included, too many patients who have believed that they were seeing a 'specialist' who was nothing more than a general surgeon who does a lot of colon/rectal surgeries. I'm not implying that that is necessarily a negative thing, BUT....remember that the pelvis is a tight space and, again IMO, needs a specialist....one who has undergone extensive training and one who ONLY operates on the colon/rectum.
You certainly can start out with a surgeon who will almost certainly refer you to an oncologist to get all the testing started although he/she (surgeon) may refer you for the ultrasound. You should also realize that in most cases, you won't actually be dealing with the surgeon until after chemoradiation is over (first he has to start....after testing...at a minimum that is a 2 week process) and after that a minimum of a 6-8 week rest period. Personally, I didn't like the surgeon that I had first met but didn't even think of looking for a second one without first seeing the onc (whom I liked) and getting started with the treatment. My point is that you have time to find a surgeon and you may not feel comfortable or have trust in the first one you see. One thing with rectal cancer is that after diagnosis, it seems to take a whole lot longer than one expected to get started. There are all the tests that need to be done before treatment (usually chemoradiation is first) and it can be very overwhelming and stressful.
Verify the surgeon(s) that you are considering. Get a referral to an oncologist (ask your GP, cousin, friends ...especially nurses) and see him/her to get started. Whichever path you choose to start on just remember that you have to feel comfortable and trust the docs that you are putting your faith in. Your oncologist will be your doctor that you see for most of the next 5-7 years so make sure you like him/her and feel comfortable with his/her judgement.
Dx 6/22/2006 IIA rectal cancer
6 wks rad/Xeloda -finished 9/06
1st attempt transanal excision 11/06
11/17/06 XELOX 1 cycle
5 months Xeloda only Dec '06 - April '07
10+ blood clots, 1 DVT 1/07
transanal excision 4/20/07 path-NO CANCER CELLS!
NED now and forever!
Perform random acts of kindness
6 wks rad/Xeloda -finished 9/06
1st attempt transanal excision 11/06
11/17/06 XELOX 1 cycle
5 months Xeloda only Dec '06 - April '07
10+ blood clots, 1 DVT 1/07
transanal excision 4/20/07 path-NO CANCER CELLS!
NED now and forever!
Perform random acts of kindness
- O Stoma Mia
- Posts: 1709
- Joined: Sat Jun 22, 2013 6:29 am
- Location: On vacation. Off-line for now.
Re: New Diagnosis/Overwhelmed
lakeswim wrote:49 - Female
DX: RC
Size: 6cm near (?) anus
Welcome to the Forum, and it's not too early for you to start posting. In fact, you can start by setting up a Signature with just the 3 lines quoted above, and then you can add more lines whenever you have new information to share.
A link for setting up a signature is here:
https://coloncancersupport.colonclub.com/viewtopic.php?f=1&t=52681&p=421597#p421597
It looks like your tumor is located about 6 cm from the anal verge (AV). If so, you can see from the diagram below roughly where it is located -- somewhere in the lower third of the rectum, but above the internal anal sphincter muscle.
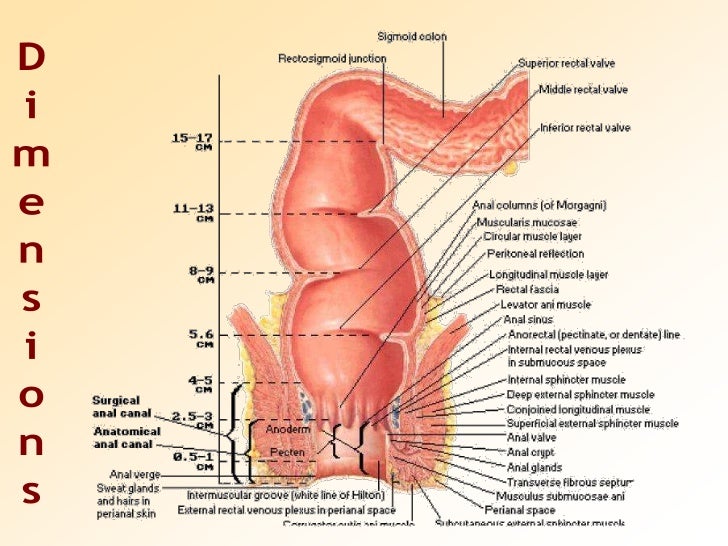
When you talk to the doctor you might also want to ask about the lateral location of the tumor, i.e. whether it is on the dorsal (back) wall of the rectum, or on the ventral (front) wall, or along the left or right side. This might make a difference, either for planning the surgery or for setting up the radiation beams. (Some tumors are located in more difficult places than others.)
Your treatment plan will be developed after they have done all the preliminary testing. If they are using the NCCN guidelines for planning, then they will probably be following the decision tree located on p. 8 (Section REC-2) of the guidelines below.
https://www.tri-kobe.org/nccn/guideline/colorectal/english/rectal.pdf
Re: New Diagnosis/Overwhelmed
Great info - thank you so much. Though I was unclear about my stats. My GI who did colonoscopy said it was large and 5-6 cm long. I understood it to be the length of the polyp - not that far from anus. I will have to ask how far it is because I’m sure that matters.
I was told this afternoon by a cancer hematologist (friend of friend) that they do surgery (resection) FIRST. And then do scans. I thought they did scans first. He told me the surgery gives them far more info than any radiology. I was surprised he said this because I have only read so far that they do lots of scans first. Anyway - more confusion.
Thanks so much for your informative reply. Good graphic too.
I was told this afternoon by a cancer hematologist (friend of friend) that they do surgery (resection) FIRST. And then do scans. I thought they did scans first. He told me the surgery gives them far more info than any radiology. I was surprised he said this because I have only read so far that they do lots of scans first. Anyway - more confusion.
Thanks so much for your informative reply. Good graphic too.
Female - RC dgns @ 49 y
Adenocarcinoma
10-11 cm from anal verge ("large")
Stage 3a - T4N0M0
FOLFOX May -Sept 18
Capecetabine + Radiation - 28 sessions - Oct - Nov 18
Jan 19 - MRI & flex sig show tumor gone, Chest/ab CT no change
Feb 19 - MRI & flex sig show tumor gone
W&W (must travel)
.....W&W surveillance 2019,2020,2021,2022,2023....
Jan 24 - approaching 5 years this Spring with W&W surveillance to end.
*grateful*
Adenocarcinoma
10-11 cm from anal verge ("large")
Stage 3a - T4N0M0
FOLFOX May -Sept 18
Capecetabine + Radiation - 28 sessions - Oct - Nov 18
Jan 19 - MRI & flex sig show tumor gone, Chest/ab CT no change
Feb 19 - MRI & flex sig show tumor gone
W&W (must travel)
.....W&W surveillance 2019,2020,2021,2022,2023....
Jan 24 - approaching 5 years this Spring with W&W surveillance to end.
*grateful*
Re: New Diagnosis/Overwhelmed
lakeswim wrote:Great info - thank you so much. Though I was unclear about my stats. My GI who did colonoscopy said it was large and 5-6 cm long. I understood it to be the length of the polyp - not that far from anus. I will have to ask how far it is because I’m sure that matters.
I was told this afternoon by a cancer hematologist (friend of friend) that they do surgery (resection) FIRST. And then do scans. I thought they did scans first. He told me the surgery gives them far more info than any radiology. I was surprised he said this because I have only read so far that they do lots of scans first. Anyway - more confusion.
Thanks so much for your informative reply. Good graphic too.
The standard of care for rectal cancer is to have chemoradiation first, then surgery, then adjuvant chemotherapy, and finally reversal of the ostomy if at all possible. There are some research studies going on right now that do a total neoadjuvant approach, which would mean all chemotherapy and/or radiation treatment before surgery, but that is not the standard of care, yet. You can read the NCCN guidelines for the treatment of rectal cancer here: https://www.nccn.org/patients/guideline ... rectal.pdf This booklet also has some suggested questions for you to ask your doctors.
When I was diagnosed, my gastroenterologist referred me to a colorectal surgeon and referred me for my first CT scan. The colorectal surgeon examined me and performed the endorectal ultrasound. Based on the ultrasound, he told me I was a "working stage III," since staging can't truly be done until surgery. He then told me that I would not be seeing him for a while, because I was being referred to a medical oncologist and a radiation oncologist to begin chemoradiation treatment to shrink the tumor before surgery.
It's good that you are gathering as much information as you can now, and asking a ton of questions. Keep at it, you are your own best advocate. If you feel at all uncomfortable with a doctor, get a second opinion. I was lucky, I liked my entire team and they gave me top-notch care.
Anne, 40
Stage IIIB Rectal Cancer
T3N1bM0
2/21/17 Dx, Age 39
2/21/17 CEA 0.9
3/23/17 - 5/2/17 Chemoradiation, 28 treatments
6/14/17 Robotic LAR w/temp loop ileostomy, ovaries & fallopian tubes removed, 2/21 lymph nodes positive
7/24/17 - 12/18/17 CapeOx, 6 Cycles
7/24/17 Dx w/ovarian cancer
9/6/17 CA 125 11.1
11/27/17 CEA 2.6
12/5/17 CT NED
12/13/17 CEA 2.9
1/11/18 CA 125 8.6
1/23/18 Reversal
3/21/18 CT enlarged thymus
4/6/18 PET NED
7/10/18 CT NED
7/11/18 CEA 2.6
9/18 Bilateral Prophylactic Mastectomy
Stage IIIB Rectal Cancer
T3N1bM0
2/21/17 Dx, Age 39
2/21/17 CEA 0.9
3/23/17 - 5/2/17 Chemoradiation, 28 treatments
6/14/17 Robotic LAR w/temp loop ileostomy, ovaries & fallopian tubes removed, 2/21 lymph nodes positive
7/24/17 - 12/18/17 CapeOx, 6 Cycles
7/24/17 Dx w/ovarian cancer
9/6/17 CA 125 11.1
11/27/17 CEA 2.6
12/5/17 CT NED
12/13/17 CEA 2.9
1/11/18 CA 125 8.6
1/23/18 Reversal
3/21/18 CT enlarged thymus
4/6/18 PET NED
7/10/18 CT NED
7/11/18 CEA 2.6
9/18 Bilateral Prophylactic Mastectomy
- O Stoma Mia
- Posts: 1709
- Joined: Sat Jun 22, 2013 6:29 am
- Location: On vacation. Off-line for now.
Re: New Diagnosis/Overwhelmed
It's good that you are collecting lots of information now, because this will allow you to be better informed and in a better position to participate in the decision-making process.
If your cancer is a polyp but not yet a tumor, then it will be a different page of the NCCN guidelines that they will be using, and a different set of questions to answer. I think the decision tree on polyps is on page 7 of the guidelines, in Section REC-1. There are two main kinds of polyps, 'sessile' (flat) polyps, and 'pedunculated' polyps (ones like a mushroom, with a stalk). These are handled differently according to different procedures. You need to find out which kind of polyp it is, because the removal procedures are different. You should also get a printed copy of your colonoscopy report (and the biopsy report) because these will have the information you need.
You may also want to have a look at this old post below. It might have some information that could help you clarify your situation.
http://coloncancersupport.colonclub.com/viewtopic.php?f=1&t=53147&p=419990#p419990
If your cancer is a polyp but not yet a tumor, then it will be a different page of the NCCN guidelines that they will be using, and a different set of questions to answer. I think the decision tree on polyps is on page 7 of the guidelines, in Section REC-1. There are two main kinds of polyps, 'sessile' (flat) polyps, and 'pedunculated' polyps (ones like a mushroom, with a stalk). These are handled differently according to different procedures. You need to find out which kind of polyp it is, because the removal procedures are different. You should also get a printed copy of your colonoscopy report (and the biopsy report) because these will have the information you need.
You may also want to have a look at this old post below. It might have some information that could help you clarify your situation.
http://coloncancersupport.colonclub.com/viewtopic.php?f=1&t=53147&p=419990#p419990
O Stoma Mia wrote:With rectal cancer, the stage and location of the tumor/polyp are very important and ultimately determine the treatment plan.
The rectum is about 15 cm long and can be divided roughly into three equal parts: low-rectum, mid-rectum, and upper-rectum. It is very important to know exactly where the tumor is located. The surgeon will have to remove the tumor/polyp and leave at least 2cm of clear margin below it. If the tumor/polyp is already very close to the sphincter, then this poses a problem for a sphincter saving operation (SSO).
It is very important to line up the best board-certified rectal surgeon that you can find, because you will want to have a surgeon who has had a lot of experience with successful sphincter-saving operations.
The main options for treatment are shown below, and depend on the T value (tumor invasion level), the stage, and the location of the tumor within the rectum. The decision process is a bit complicated, so you need to have a very experienced rectal cancer surgeon who can properly evaluate all of the available options and choose the best option for you.
FIGURE 30-3. Treatment options for rectal cancer depending on stage and location.
Reference: The ASCRS Textbook of Colon and Rectal Surgery: Second Edition, 2011, Surgical Treatment of Rectal Cancer, Chapter 30. p. 421
Treatment options for rectal cancer depending on stage and locationReference: http://www.springer.com/cda/content/document/cda_downloaddocument/9780387248462-c30.pdf
- Stage I (T1N0, T2N0—The cancer is confined to the rectal wall and no nodes are involved)
● Distal rectal cancers: T1 (invasion into the submucosa only)■ Local excision
● Distal rectal cancers: T2 (invasion into the muscularis propria)
■ Radical resection, often an APR
■ Adjuvant therapy is usually not recommended.■ Local excision with preoperative or postoperative adjuvant therapy
● Mid rectal cancer: T1
■ Radical resection without adjuvant therapy, often an APR■ TEM
● Mid rectal cancer: T2
■ Radical resection, usually an LAR with low anastomosis. A temporary proximal diverting ostomy is often required.
■ Adjuvant therapy is usually not recommended.■ TEM with either preoperative or postoperative adjuvant therapy
● Upper rectal cancers: T1 and T2
■ Radical resection similar to a T1 cancer
■ Adjuvant therapy is not recommended if a radical resection is performed but is recommended after a TEM resection.■ LAR
- Stage II and Stage III cancers [Stage II cancers have invasion into the mesorectal fat (T3) but no involved mesorectal lymph nodes. Stage III cancers are any rectal cancer (T1, T2, or T3) but with involved lymph nodes.]
● Distal rectal cancers■ Preoperative adjuvant therapy is most often recommended followed by a radical resection, usually an APR.
● Mid rectal cancers
■ If preoperative imaging does not clearly define the stage of the cancer, resection can be done first followed by postoperative adjuvant
therapy.■ Same as above for distal rectal cancers except an LAR is usually performed instead of an APR.
● Upper rectal cancers■ LAR, with either preoperative or postoperative adjuvant therapy
- Stage IV cancers
● Treatment for any cancer is dependent on the extent of metastasis. With better surgical and medical treatments for metastatic disease,
locoregional control of the primary should be aggressive and similar to the above recommendations except in the most advanced cases.
(Key: LE, local excision; short XRT, short-course radiation therapy given 2 times a day for 5 days in larger fractions; ChXRT, long-course
therapy given in 30 smaller fractions over 6 weeks in combination with chemotherapy)
Re: New Diagnosis/Overwhelmed
My tumor was 5.2 cm so a little smaller than yours but considered
large. The size resulted in some rather difficult bathroom problems
and I was worried that I would get a blockage so I was in a pretty big
hurry to get started with treatment. The tumor started getting smaller
about three weeks into chemo + radiation. I couldn't understand why
they didn't just cut it out but I didn't realize how technically
complicated it was to remove a rectal tumor safely.
My GI guy referred me to a local oncologist and radiologist. I then
got second opinions at Dana Farber Cancer Institute (a major cancer
center in Boston) and picked a surgeon at Brigham and Women's Hospital
in Boston (they do the cancer surgeries for Dana Farber). My surgeon
was a CRC board certified surgeon and highly qualified. I posted a
link to a research study showing better outcomes (in terms of fewer
recurrences) at major cancer centers a while ago.
You can switch gears between doctors. I have interleaved some doctors
appointments between hospitals.
The process at major cancer centers can be quite challenging. I was
able to get an immediate appointment at my local hospital. It took me
two weeks to get appointments at Dana Farber and Brigham and Womens. I
found out why when I visited the place. They do an incredible amount
of volume and you're pipelined though administrative staff before you
get to the doctors. At my local hospital, there's one waiting room and
the number of people there is usally small and this waiting room was
for all kinds of cancer. When I went for my oncology appointment at
Dana Farber, I went into a room that could probably hold over 100
patients and that room was just for Colorectal patients. They had a
number of CRC oncologists at Dana Farber. They had one oncologist for
all cancers at my local hospital. They now have two as they hired
another one recently.
So there may be more of the feeling of being treated like a number at
a major cancer center but the level of expertise goes way up because
of specialization.
When I had my surgery, the vast majority of other patients coming in
for surgery had suitcases (I brought a small duffel bag). So it seemed
to me that a lot of people had traveled for surgical services. The major
cancer centers in Boston (Mass General Hospital and Dana Farber/Brigham
and Women's) get a lot of business from people in other states and
other countries. You might do as I did and get radiation and chemo
locally and surgical services from a major cancer center as a means
to minimize travel and time spent in hotels for caregivers.
There is a month to six weeks between Neo-Adjuvant Chemo/Radiation
and surgery and that gives the body time to heal. During that time
I ran, worked, and played tennis. I felt quite good after the
radiation effects wore off. If you're in generally good shape, you
should be okay to travel. On the day before surgery, I drove to my
mother's house, left my car there, took a 75 minute ride on the
subway to get to the hospital, checked into a hotel and did a lot
of walking. There was a tropical storm at the time so walking
outside meant getting quite wet.
You can feel quite challenged after surgery though. Your body
will likely be weak and you'll have to deal with the illeostomy
bag and the hospital will want you back in two weeks for the
post-surgical checkup and they will see how you're doing with the
bag. The WOC nurses at Brigham and Women's were very good and far
better than the visiting nurses locally. I asked them to order
illeostomy bags for me and gave them the brand and size and they
ordered me colostomy bags. I was not impressed nor was I happy
that I'd have to return the bags and then wait for the right ones
to be shipped.
On talking to the insurance company - I never contacted them outside
of looking on their web portal. I did check what their coverage was
for various hospitals and the two major cancer centers in Boston.
They basically just paid their portion of the bills and I had bills
for what they didn't cover. I paid the out-of-pocket max last year
and I will pay it again this year.
I think that it wouldn't be a bad idea to ensure that your covered for
major costs. My insurance company did offer some concierge services in
setting me up for services but this was after I had everything already
set up.
If you're traveling a long distance, then it might be more efficient
if you have a relative nearby that could house you for about three
weeks so that you can make the post-op meeting. There may be additional
meetings later on. I had a five-month checkup and there will be the
additional surgery to do the illeostomy reversal. That will have a
three-four night hospital stay.
So travel does present challenges but I did travel for the surgical
part and I would definitely do it again.
On proximity - my tumor actually popped outside a few times so mine
was also fairly low but I had 90% shrinkage of the tumor from chemo
and radiation so the margin situation might be a lot better after
your initial treatment.
large. The size resulted in some rather difficult bathroom problems
and I was worried that I would get a blockage so I was in a pretty big
hurry to get started with treatment. The tumor started getting smaller
about three weeks into chemo + radiation. I couldn't understand why
they didn't just cut it out but I didn't realize how technically
complicated it was to remove a rectal tumor safely.
My GI guy referred me to a local oncologist and radiologist. I then
got second opinions at Dana Farber Cancer Institute (a major cancer
center in Boston) and picked a surgeon at Brigham and Women's Hospital
in Boston (they do the cancer surgeries for Dana Farber). My surgeon
was a CRC board certified surgeon and highly qualified. I posted a
link to a research study showing better outcomes (in terms of fewer
recurrences) at major cancer centers a while ago.
You can switch gears between doctors. I have interleaved some doctors
appointments between hospitals.
The process at major cancer centers can be quite challenging. I was
able to get an immediate appointment at my local hospital. It took me
two weeks to get appointments at Dana Farber and Brigham and Womens. I
found out why when I visited the place. They do an incredible amount
of volume and you're pipelined though administrative staff before you
get to the doctors. At my local hospital, there's one waiting room and
the number of people there is usally small and this waiting room was
for all kinds of cancer. When I went for my oncology appointment at
Dana Farber, I went into a room that could probably hold over 100
patients and that room was just for Colorectal patients. They had a
number of CRC oncologists at Dana Farber. They had one oncologist for
all cancers at my local hospital. They now have two as they hired
another one recently.
So there may be more of the feeling of being treated like a number at
a major cancer center but the level of expertise goes way up because
of specialization.
When I had my surgery, the vast majority of other patients coming in
for surgery had suitcases (I brought a small duffel bag). So it seemed
to me that a lot of people had traveled for surgical services. The major
cancer centers in Boston (Mass General Hospital and Dana Farber/Brigham
and Women's) get a lot of business from people in other states and
other countries. You might do as I did and get radiation and chemo
locally and surgical services from a major cancer center as a means
to minimize travel and time spent in hotels for caregivers.
There is a month to six weeks between Neo-Adjuvant Chemo/Radiation
and surgery and that gives the body time to heal. During that time
I ran, worked, and played tennis. I felt quite good after the
radiation effects wore off. If you're in generally good shape, you
should be okay to travel. On the day before surgery, I drove to my
mother's house, left my car there, took a 75 minute ride on the
subway to get to the hospital, checked into a hotel and did a lot
of walking. There was a tropical storm at the time so walking
outside meant getting quite wet.
You can feel quite challenged after surgery though. Your body
will likely be weak and you'll have to deal with the illeostomy
bag and the hospital will want you back in two weeks for the
post-surgical checkup and they will see how you're doing with the
bag. The WOC nurses at Brigham and Women's were very good and far
better than the visiting nurses locally. I asked them to order
illeostomy bags for me and gave them the brand and size and they
ordered me colostomy bags. I was not impressed nor was I happy
that I'd have to return the bags and then wait for the right ones
to be shipped.
On talking to the insurance company - I never contacted them outside
of looking on their web portal. I did check what their coverage was
for various hospitals and the two major cancer centers in Boston.
They basically just paid their portion of the bills and I had bills
for what they didn't cover. I paid the out-of-pocket max last year
and I will pay it again this year.
I think that it wouldn't be a bad idea to ensure that your covered for
major costs. My insurance company did offer some concierge services in
setting me up for services but this was after I had everything already
set up.
If you're traveling a long distance, then it might be more efficient
if you have a relative nearby that could house you for about three
weeks so that you can make the post-op meeting. There may be additional
meetings later on. I had a five-month checkup and there will be the
additional surgery to do the illeostomy reversal. That will have a
three-four night hospital stay.
So travel does present challenges but I did travel for the surgical
part and I would definitely do it again.
On proximity - my tumor actually popped outside a few times so mine
was also fairly low but I had 90% shrinkage of the tumor from chemo
and radiation so the margin situation might be a lot better after
your initial treatment.
6/17: ER rectal bleeding; Colonoscopy
7/17: 3B rectal. T3N1bM0. 5.2 4.5 4.3 cm. Lymphs: 6 x 4 mm, 8 x 6, 5 x 5
7/17-9/17: Xeloda radiation
7/5: CEA 2.7; 8/16: 1.9; 11/30: 0.6; 12/20 1.4; 1/10 1.8; 1/31 2.2; 2/28 2.6; 4/10 2.8; 5/1 2.8; 5/29 3.2; 7/13 4.5; 8/9 2.8, 2/12 1.2
MSS, KRAS G12D
10/17: 2.7 2.2 1.6 cm (-90%). Lymphs: 3 x 3 mm (-62.5%), 4 x 3 (-75%), 5 x 3 (-40%). 5.1 CM from AV
10/17: LAR, Temp Ileostomy, Path Complete Response
CapeOx (8) 12/17-6/18
7/18: Reversal, Port Removal
2/19: Clean CT
7/17: 3B rectal. T3N1bM0. 5.2 4.5 4.3 cm. Lymphs: 6 x 4 mm, 8 x 6, 5 x 5
7/17-9/17: Xeloda radiation
7/5: CEA 2.7; 8/16: 1.9; 11/30: 0.6; 12/20 1.4; 1/10 1.8; 1/31 2.2; 2/28 2.6; 4/10 2.8; 5/1 2.8; 5/29 3.2; 7/13 4.5; 8/9 2.8, 2/12 1.2
MSS, KRAS G12D
10/17: 2.7 2.2 1.6 cm (-90%). Lymphs: 3 x 3 mm (-62.5%), 4 x 3 (-75%), 5 x 3 (-40%). 5.1 CM from AV
10/17: LAR, Temp Ileostomy, Path Complete Response
CapeOx (8) 12/17-6/18
7/18: Reversal, Port Removal
2/19: Clean CT
Re: New Diagnosis/Overwhelmed
Thank you all so much. These posts are so informative - yet make my brain swim.
I just logged on to my GI doc’s site and found some info.
Rectum, adenocarcinoma, poorly differentiated. (I just read that this last part is bad news?!?!.).
Does NOT say where in rectum exactly!
Then lots of clinical info about proteins and staining and sizes of tissue fragments submitted.
Thank you...
I just logged on to my GI doc’s site and found some info.
Rectum, adenocarcinoma, poorly differentiated. (I just read that this last part is bad news?!?!.).
Does NOT say where in rectum exactly!
Then lots of clinical info about proteins and staining and sizes of tissue fragments submitted.
Thank you...
Female - RC dgns @ 49 y
Adenocarcinoma
10-11 cm from anal verge ("large")
Stage 3a - T4N0M0
FOLFOX May -Sept 18
Capecetabine + Radiation - 28 sessions - Oct - Nov 18
Jan 19 - MRI & flex sig show tumor gone, Chest/ab CT no change
Feb 19 - MRI & flex sig show tumor gone
W&W (must travel)
.....W&W surveillance 2019,2020,2021,2022,2023....
Jan 24 - approaching 5 years this Spring with W&W surveillance to end.
*grateful*
Adenocarcinoma
10-11 cm from anal verge ("large")
Stage 3a - T4N0M0
FOLFOX May -Sept 18
Capecetabine + Radiation - 28 sessions - Oct - Nov 18
Jan 19 - MRI & flex sig show tumor gone, Chest/ab CT no change
Feb 19 - MRI & flex sig show tumor gone
W&W (must travel)
.....W&W surveillance 2019,2020,2021,2022,2023....
Jan 24 - approaching 5 years this Spring with W&W surveillance to end.
*grateful*
Re: New Diagnosis/Overwhelmed
First, thank you for all this info. It's incredible but my head is swimming.I need to print all of this out and highlight.
Second, I'm starting to freak out more because I now see things with different eyes. The weird sensation I was used to in my anus that I was told was a skin tag (by the first Rectal Surgeon who told me I had anal fissure - after a rectal exam) and also a hemorrhoid (that I keep tucking back in) by my GYN office - I'm thinking this must be the polyp (tumor? what's the difference?). It's right there around my sphinctor - and it does give me a full feeling at times. So I am thinking I am going to need a surgeon who is well-versed in sphincter saving strategies (if even possible, if this is indeed where it is) and I'm thinking I need to get this process going ASAP, given the location. I wonder if anyone here knows of any better sphincted saving surgeons.
Also, the back pain I've been experiencing for the last year? I now realize is radiates from that area in my bottom where the lump is in my anus. Which is probably not good news either. This has all been pretty nonspecific and I've had reasons for all of it (dog pulled me down for my back), docs told me hemorrhoid/anal fissure - so I have written it all off until now. The feeling around the anus also seems more pronounced since the colonoscopy - as if they accelerated it or at least moved things around. I don't know.
As for travel, the info about traveling and scheduling and insurance is all good. Should I schedule something now with a big cancer center - instead of after my surgeon visit here in Rochester - so I don't have to wait as long? Like I mentioned, I have relatives within an hour or two of both Hopkins, Philly, and NYC. But to get to those places, it is >5 hours from my home and my kids.
Also, I was told by my GYN office nurse that I can't change surgeons (to another on the same team) once I meet with them. I find this hard to believe. I have changed PCP and am seeing a new one tomorrow morning (he is associated with the better hospital in this area) and will ask him.
Lastly, my previous post with this info appears to be lost but I found more info on my online chart. Doesn't specify where tumor is (though I may know already) but says the following..... I guess "poorly differentiated" is a very negative thing, based on my online research.
Also, I will work on my signature after my Thursday appointment - once I know more. Thank you for the link for that.
>>>>
(B) Rectum, mass, biopsy:
- Adenocarcinoma, poorly differentiated.
Immunohistochemical stains for the mismatch repair proteins MLH1, MSH2,
MSH6 and PMS2 were performed. The tumor cells demonstrate retained
nuclear staining for all four proteins, indicating the tumor is MMR
proficient (pMMR) and likely microsatellite stable.
Thank you so much.
Susan
49 - RC
More info to come!
Second, I'm starting to freak out more because I now see things with different eyes. The weird sensation I was used to in my anus that I was told was a skin tag (by the first Rectal Surgeon who told me I had anal fissure - after a rectal exam) and also a hemorrhoid (that I keep tucking back in) by my GYN office - I'm thinking this must be the polyp (tumor? what's the difference?). It's right there around my sphinctor - and it does give me a full feeling at times. So I am thinking I am going to need a surgeon who is well-versed in sphincter saving strategies (if even possible, if this is indeed where it is) and I'm thinking I need to get this process going ASAP, given the location. I wonder if anyone here knows of any better sphincted saving surgeons.
Also, the back pain I've been experiencing for the last year? I now realize is radiates from that area in my bottom where the lump is in my anus. Which is probably not good news either. This has all been pretty nonspecific and I've had reasons for all of it (dog pulled me down for my back), docs told me hemorrhoid/anal fissure - so I have written it all off until now. The feeling around the anus also seems more pronounced since the colonoscopy - as if they accelerated it or at least moved things around. I don't know.
As for travel, the info about traveling and scheduling and insurance is all good. Should I schedule something now with a big cancer center - instead of after my surgeon visit here in Rochester - so I don't have to wait as long? Like I mentioned, I have relatives within an hour or two of both Hopkins, Philly, and NYC. But to get to those places, it is >5 hours from my home and my kids.
Also, I was told by my GYN office nurse that I can't change surgeons (to another on the same team) once I meet with them. I find this hard to believe. I have changed PCP and am seeing a new one tomorrow morning (he is associated with the better hospital in this area) and will ask him.
Lastly, my previous post with this info appears to be lost but I found more info on my online chart. Doesn't specify where tumor is (though I may know already) but says the following..... I guess "poorly differentiated" is a very negative thing, based on my online research.
Also, I will work on my signature after my Thursday appointment - once I know more. Thank you for the link for that.
>>>>
(B) Rectum, mass, biopsy:
- Adenocarcinoma, poorly differentiated.
Immunohistochemical stains for the mismatch repair proteins MLH1, MSH2,
MSH6 and PMS2 were performed. The tumor cells demonstrate retained
nuclear staining for all four proteins, indicating the tumor is MMR
proficient (pMMR) and likely microsatellite stable.
Thank you so much.
Susan
49 - RC
More info to come!
Female - RC dgns @ 49 y
Adenocarcinoma
10-11 cm from anal verge ("large")
Stage 3a - T4N0M0
FOLFOX May -Sept 18
Capecetabine + Radiation - 28 sessions - Oct - Nov 18
Jan 19 - MRI & flex sig show tumor gone, Chest/ab CT no change
Feb 19 - MRI & flex sig show tumor gone
W&W (must travel)
.....W&W surveillance 2019,2020,2021,2022,2023....
Jan 24 - approaching 5 years this Spring with W&W surveillance to end.
*grateful*
Adenocarcinoma
10-11 cm from anal verge ("large")
Stage 3a - T4N0M0
FOLFOX May -Sept 18
Capecetabine + Radiation - 28 sessions - Oct - Nov 18
Jan 19 - MRI & flex sig show tumor gone, Chest/ab CT no change
Feb 19 - MRI & flex sig show tumor gone
W&W (must travel)
.....W&W surveillance 2019,2020,2021,2022,2023....
Jan 24 - approaching 5 years this Spring with W&W surveillance to end.
*grateful*
-
weisssoccermom
- Posts: 5988
- Joined: Thu May 10, 2007 2:32 pm
- Location: Pacific NW
Re: New Diagnosis/Overwhelmed
I find it hard to believe that you can't switch surgeons HOWEVER, I have heard, in some very strict HMO organizations that they are not at all amenable to switching doctors so that might be the case IF that is the type of insurance you have.
What IS true, though is that if you switch to another doctor within the same practice you likely won't find a second surgeon willing to change directions from his colleague. That's not the same as saying you just prefer the personality of a different surgeon. I don't know why that nurse would have said that unless the particular surgical practice has that restriction.
As for going out of state...just wait until you get some more answers. As others have said, you certainly can go local for the chemo and radiation and may want to go elsewhere for the surgery. For example, I had all my chemo and radiation local but chose to go to Seattle for my surgery.
I don't know why that one person would have told you that they do surgery first and then scans. Even with colon cancer that generally does the surgery first, every person that I know of has at least had (unless it is an emergency) a CT/MRI FIRST before the surgery. The doctors, particularly the surgeon wants to do what he/she is dealing with before operating. While yes, it is true that the pathology helps to stage the cancer, with rectal cancer, it is a whole different scenario. When chemo or chemoradiation is given neoadjuvantally (before surgery), a CLINICAL staging must be done first. This is accomplished by doing the following tests:
a CT, MRI or PET to check for distant mets and distant/local lymph node involvement
an EUS (endorectal ultrasound....also referred to as transanal ultrasound) to determine the depth of the tumor into the rectal wall AND to verify for local nodes (more accurate than the CT, MRI or PET)
blood work.
Staging is determined by the following three factors:
T N M
The 'T' stage (not to be confused with the cancer stage) is defined as the DEPTH of rectal wall (or colon wall) involvement of the tumor
The 'N' designation is the number of nodes believed to be affected by the cancer
The 'M' stands for distant mets
With rectal cancer, the objective of the chemoradiation is to shrink the tumor and to kill off the local lymph nodes if any are affected. Staging solely by pathology would be a mute point after chemoradiation. I am a perfect example. The EUS/CT scans all showed no local lymph node involvement and no distant mets. Based on the EUS, my tumor was deemed to be a T3. After chemoradiation, there was no sign of the tumor and the pathology showed no cancer cells and no residual tumor. That doesn't mean that I was 'restaged' to not having cancer. It simply meant that the chemoradiation did its job and I had a complete pathological response...which is the objective of the treatments. So, with rectal cancer, the patient is clinically staged and REMAINS that stage even if all the tumor is zapped and destroyed by the chemoradiation.
I have no idea why that friend of a friend told you that information.....because with rectal cancer they CLINICALLY stage via all the above tests and THEN do surgery....even with the stage I patient who GENERALLY doesn't undergo chemoradiation. Even with colon cancer where patients don't get chemoradiation (the colon isn't fixed whereas the rectum is, so radiating it usually not recommended for them) I have always heard that they get scans first unless it is a true emergency to have the surgery first.
My advice....stop listening to 'friends of friends' who don't know your situation, don't have your records in front of them and shouldn't be giving out specific information without knowing everything about your case. I know it's hard, especially in the first few days, but try and relax, get yourself prepared for your appointment on Thursday and then go from there. Did you verify that this surgeon is board certified in colon/rectal surgery?
My next piece of advice is for you to go to the store, get a three ring notebook, some dividers and start your notebook by labeling the dividers......CT/MRI scans, bloodwork, pathology report, colonoscopy, etc. Next, make sure that your PCP is copied on each and every report....the prior ones (colonoscopy to start with) and all future ones as well. Next, get a hard copy of every test that you have had so far. Right now, that sounds like the only one is the colonoscopy. DO NOT just listen to what the report said from the doctor or the computer....get the actual report. Too often, you'll find that the doctors don't necessarily tell you everything that is on those reports. For example, I had a kidney stone that showed up on my first CT scan back in 2006. Pretty darn irrelevant with respect to my cancer but important to me. Really came in handy to know when 10 years later, I passed that supposedly non blocking stone!
With rectal cancer, you have to be patient....and I know that's hard. You just want it out but....the doctors first need to know exactly what they are dealing with to determine the best approach for YOU! This is accomplished by running these first tests...the CT/MRI or PET, the EUS and bloodwork. Those take some time to schedule and the wait can seem like forever...even if it is only a few days. Then IF it is recommended, you will start radiation but first, you have to see a radiation oncologist, set up the initial appointment with him/her and then go for the simulation appointment to get those treatments planned out before you actually start. Again, that wait....even if it is only a few days, can seem to take forever. Concentrate now on getting other things done....as silly as it sounds, get any dental work done, get any special projects done around the house (presuming they are small) and try to relax.
What IS true, though is that if you switch to another doctor within the same practice you likely won't find a second surgeon willing to change directions from his colleague. That's not the same as saying you just prefer the personality of a different surgeon. I don't know why that nurse would have said that unless the particular surgical practice has that restriction.
As for going out of state...just wait until you get some more answers. As others have said, you certainly can go local for the chemo and radiation and may want to go elsewhere for the surgery. For example, I had all my chemo and radiation local but chose to go to Seattle for my surgery.
I don't know why that one person would have told you that they do surgery first and then scans. Even with colon cancer that generally does the surgery first, every person that I know of has at least had (unless it is an emergency) a CT/MRI FIRST before the surgery. The doctors, particularly the surgeon wants to do what he/she is dealing with before operating. While yes, it is true that the pathology helps to stage the cancer, with rectal cancer, it is a whole different scenario. When chemo or chemoradiation is given neoadjuvantally (before surgery), a CLINICAL staging must be done first. This is accomplished by doing the following tests:
a CT, MRI or PET to check for distant mets and distant/local lymph node involvement
an EUS (endorectal ultrasound....also referred to as transanal ultrasound) to determine the depth of the tumor into the rectal wall AND to verify for local nodes (more accurate than the CT, MRI or PET)
blood work.
Staging is determined by the following three factors:
T N M
The 'T' stage (not to be confused with the cancer stage) is defined as the DEPTH of rectal wall (or colon wall) involvement of the tumor
The 'N' designation is the number of nodes believed to be affected by the cancer
The 'M' stands for distant mets
With rectal cancer, the objective of the chemoradiation is to shrink the tumor and to kill off the local lymph nodes if any are affected. Staging solely by pathology would be a mute point after chemoradiation. I am a perfect example. The EUS/CT scans all showed no local lymph node involvement and no distant mets. Based on the EUS, my tumor was deemed to be a T3. After chemoradiation, there was no sign of the tumor and the pathology showed no cancer cells and no residual tumor. That doesn't mean that I was 'restaged' to not having cancer. It simply meant that the chemoradiation did its job and I had a complete pathological response...which is the objective of the treatments. So, with rectal cancer, the patient is clinically staged and REMAINS that stage even if all the tumor is zapped and destroyed by the chemoradiation.
I have no idea why that friend of a friend told you that information.....because with rectal cancer they CLINICALLY stage via all the above tests and THEN do surgery....even with the stage I patient who GENERALLY doesn't undergo chemoradiation. Even with colon cancer where patients don't get chemoradiation (the colon isn't fixed whereas the rectum is, so radiating it usually not recommended for them) I have always heard that they get scans first unless it is a true emergency to have the surgery first.
My advice....stop listening to 'friends of friends' who don't know your situation, don't have your records in front of them and shouldn't be giving out specific information without knowing everything about your case. I know it's hard, especially in the first few days, but try and relax, get yourself prepared for your appointment on Thursday and then go from there. Did you verify that this surgeon is board certified in colon/rectal surgery?
My next piece of advice is for you to go to the store, get a three ring notebook, some dividers and start your notebook by labeling the dividers......CT/MRI scans, bloodwork, pathology report, colonoscopy, etc. Next, make sure that your PCP is copied on each and every report....the prior ones (colonoscopy to start with) and all future ones as well. Next, get a hard copy of every test that you have had so far. Right now, that sounds like the only one is the colonoscopy. DO NOT just listen to what the report said from the doctor or the computer....get the actual report. Too often, you'll find that the doctors don't necessarily tell you everything that is on those reports. For example, I had a kidney stone that showed up on my first CT scan back in 2006. Pretty darn irrelevant with respect to my cancer but important to me. Really came in handy to know when 10 years later, I passed that supposedly non blocking stone!
With rectal cancer, you have to be patient....and I know that's hard. You just want it out but....the doctors first need to know exactly what they are dealing with to determine the best approach for YOU! This is accomplished by running these first tests...the CT/MRI or PET, the EUS and bloodwork. Those take some time to schedule and the wait can seem like forever...even if it is only a few days. Then IF it is recommended, you will start radiation but first, you have to see a radiation oncologist, set up the initial appointment with him/her and then go for the simulation appointment to get those treatments planned out before you actually start. Again, that wait....even if it is only a few days, can seem to take forever. Concentrate now on getting other things done....as silly as it sounds, get any dental work done, get any special projects done around the house (presuming they are small) and try to relax.
Dx 6/22/2006 IIA rectal cancer
6 wks rad/Xeloda -finished 9/06
1st attempt transanal excision 11/06
11/17/06 XELOX 1 cycle
5 months Xeloda only Dec '06 - April '07
10+ blood clots, 1 DVT 1/07
transanal excision 4/20/07 path-NO CANCER CELLS!
NED now and forever!
Perform random acts of kindness
6 wks rad/Xeloda -finished 9/06
1st attempt transanal excision 11/06
11/17/06 XELOX 1 cycle
5 months Xeloda only Dec '06 - April '07
10+ blood clots, 1 DVT 1/07
transanal excision 4/20/07 path-NO CANCER CELLS!
NED now and forever!
Perform random acts of kindness
Return to “Colon Talk - Colon cancer (colorectal cancer) support forum”
Who is online
Users browsing this forum: No registered users and 34 guests
